Kinh Nghiệm Hướng dẫn A patient who has diabetes states that he prefers to be drawn on the inside of his wrist Chi Tiết
You đang tìm kiếm từ khóa A patient who has diabetes states that he prefers to be drawn on the inside of his wrist được Update vào lúc : 2022-10-30 05:35:20 . Với phương châm chia sẻ Mẹo Hướng dẫn trong nội dung bài viết một cách Chi Tiết 2022. Nếu sau khi tìm hiểu thêm Post vẫn ko hiểu thì hoàn toàn có thể lại phản hồi ở cuối bài để Admin lý giải và hướng dẫn lại nha.The information given here supplements that given in Chapter 2. Users of these guidelines should read Chapter 2 before reading the information given below. This chapter covers background information (Section 7.1), practical guidance (Section 7.2) and illustrations (Section 7.3) relevant to capillary sampling.
Nội dung chính Show- 7.1. Background information on capillary sampling
- 7.1.1. Choice of site
- 7.1.2. Selecting the length of lancet
- 7.1.3. Order of draw
- 7.1.4. Complications
- 7.2. Practical guidance on capillary sampling
- 7.2.1. Selection of site and lancet
- 7.2.2. Procedure for capillary sampling
- 7.3. Illustrations for capillary sampling
- Figure 7.1Capillary sampling
- What antiseptic should the phlebotomy technician use to collect a blood culture?
- Which of the following action should I phlebotomy technician take when preparing a peripheral blood smear?
- Which of the following should be the first step before entering a patient's room to perform a blood collection?
- Which of the following action by a phlebotomy technician can result in a grossly Hemolyzed specimen?
Capillary sampling from a finger, heel or (rarely) an ear lobe may be performed on patients of any age, for specific tests that require small quantities of blood. However, because the procedure is commonly used in paediatric patients, Sections 7.1.1 and 7.1.2 focus particularly on paediatric capillary sampling.
7.1. Background information on capillary sampling
7.1.1. Choice of site
Adult patientsThe finger is usually the preferred site for capillary testing in an adult patient. The sides of the heel are only used in paediatric and neonatal patients. Ear lobes are sometimes used in mass screening or research studies.
Paediatric and neonatal patientsSelection of a site for capillary sampling in a paediatric patient is usually based on the age and weight of the patient. If the child is walking, the child's feet may have calluses that hinder adequate blood flow. Table 7.1 shows the conditions influencing the choice of heel or finger-prick.
Table 7.1Conditions influencing the choice of heel or finger-prick.
Specimens requiring a skin puncture are best obtained after ensuring that a baby is warm, as discussed in Section 6.2.2.
7.1.2. Selecting the length of lancet
Adult patientsA lancet slightly shorter than the estimated depth needed should be used because the pressure compresses the skin; thus, the puncture depth will be slightly deeper than the lancet length. In one study of 52 subjects, pain increased with penetration depth, and thicker lancets were slightly more painful than thin ones (67). However, blood volumes increased with the lancet penetration and depth.
Lengths vary by manufacturer (from 0.85 mm for neonates up to 2.2 mm). In a finger-prick, the depth should not go beyond 2.4 mm, so a 2.2 mm lancet is the longest length typically used.
Paediatric and neonatal patientsIn heel-pricks, the depth should not go beyond 2.4 mm. For premature neonates, a 0.85 mm lancet is available.
The distance for a 7 pound (3 kg) baby from outer skin surface to bone is:
medial and lateral heel – 3.32 mm;
posterior heel – 2.33 mm (this site should be avoided, to reduce the risk of hitting bone);
toe – 2.19 mm.
The recommended depth for a finger-prick is:
for a child over 6 months and below 8 years – 1.5 mm;
for a child over 8 years – 2.4 mm.
Too much compression should be avoided, because this may cause a deeper puncture than is needed to get good flow.
7.1.3. Order of draw
With skin punctures, the haematology specimen is collected first, followed by the chemistry and blood bank specimens. This order of drawing is essential to minimize the effects of platelet clumping. The order used for skin punctures is the reverse of that used for venepuncture collection. If more than two specimens are needed, venepuncture may provide more accurate laboratory results.
7.1.4. Complications
Complications that can arise in capillary sampling include:
collapse of veins if the tibial artery is lacerated from puncturing the medial aspect of the heel;
osteomyelitis of the heel bone (calcaneus) (68);
nerve damage if the fingers of neonates are punctured (69);
haematoma and loss of access to the venous branch used;
scarring;
localized or generalized necrosis (a long-term effect);
skin breakdown from repeated use of adhesive strips (particularly in very young or very elderly patients) – this can be avoided if sufficient pressure is applied and the puncture site is observed after the procedure.
7.2. Practical guidance on capillary sampling
7.2.1. Selection of site and lancet
Using the guidance given in Section 7.1, decide whether to use a finger or heel-prick, and decide on an appropriate size of lancet.
DO NOT use a surgical blade to perform a skin puncture.
DO NOT puncture the skin more than once with the same lancet, or use a single puncture site more than once, because this can lead to bacterial contamination and infection.
7.2.2. Procedure for capillary sampling
Adult patientsPrepare the skinApply alcohol to the entry site and allow to air dry (see Section 2.2.3).
Puncture the skin with one quick, continuous and deliberate stroke, to achieve a good flow of blood and to prevent the need to repeat the puncture.
Wipe away the first drop of blood because it may be contaminated with tissue fluid or debris (sloughing skin).
Avoid squeezing the finger or heel too tightly because this dilutes the specimen with tissue fluid (plasma) and increases the probability of haemolysis (60).
When the blood collection procedure is complete, apply firm pressure to the site to stop the bleeding.
With skin punctures, collect the specimens in the order below, starting with haematology specimens:
–haematology specimens;
–chemistry specimens;
–blood bank specimens.
First immobilize the child by asking the parent to:
–sit on the phlebotomy chair with the child on the parent's lap;
–immobilize the child's lower extremities by positioning their legs around the child's in a cross-leg pattern;
–extend an arm across the child's chest, and secure the child's không lấy phí arm by firmly tucking it under their own;
–grasp the child's elbow (i.e. the skin puncture arm), and hold it securely;
–use his or her other arm to firmly grasp the child's wrist, holding it palm down.
Prepare the skin as described above for adult patients.
DO NOT use povidone iodine for a capillary skin puncture in paediatric and neonatal patients; instead, use alcohol, as stated in the instructions for adults.
Puncture the skin
Puncture the skin as described above for adult patients.
If necessary, take the following steps to improve the ease of obtaining blood by finger-prick in paediatric and neonatal patients:
–ask the parent to rhythmically tighten and release the child's wrist, to ensure that there is sufficient flow of blood;
–keep the child warm by removing as few clothes as possible, swaddling an infant in a blanket, and having a mother or caregiver hold an infant, leaving only the extremity of the site of capillary sampling exposed.
Avoid excessive massaging or squeezing of fingers because this will cause haemolysis and impede blood flow (60).
As described above for adult patients, collect the capillary haematology specimen first, followed by the chemistry and blood bank specimens.
-
Clean up blood spills.
Collect all equipment used in the procedure, being careful to remove all items from the patient's bed or cot; to avoid accidents, DO NOT leave anything behind.
There are two separate steps to patient follow-up care – data entry (i.e. completion of requisitions), and provision of comfort and reassurance.
Data entry or completion of requisitionsRecord relevant information about the blood collection on the requisition and specimen label; such information may include:
–date of collection;
–patient name;
–patient identity number;
–unit location (nursery or hospital room number);
–test or tests requested;
–amount of blood collected (number of tubes);
–method of collection (venepuncture or skin puncture);
–phlebotomist's initials.
Show the child that you care either verbally or physically. A simple gesture is all it takes to leave the child on a positive note; for example, give verbal praise, a handshake, a fun sticker or a simple pat on the back.
A small amount of sucrose (0.012–0.12 g) is safe and effective as an analgesic for newborns undergoing venepuncture or capillary heel-pricks (70).
Unsuccessful attempts in paediatric patientsAdhere strictly to a limit on the number of times a paediatric patient may be stuck. If no satisfactory sample has been collected after two attempts, seek a second opinion to decide whether to make a further attempt, or cancel the tests.
7.3. Illustrations for capillary sampling
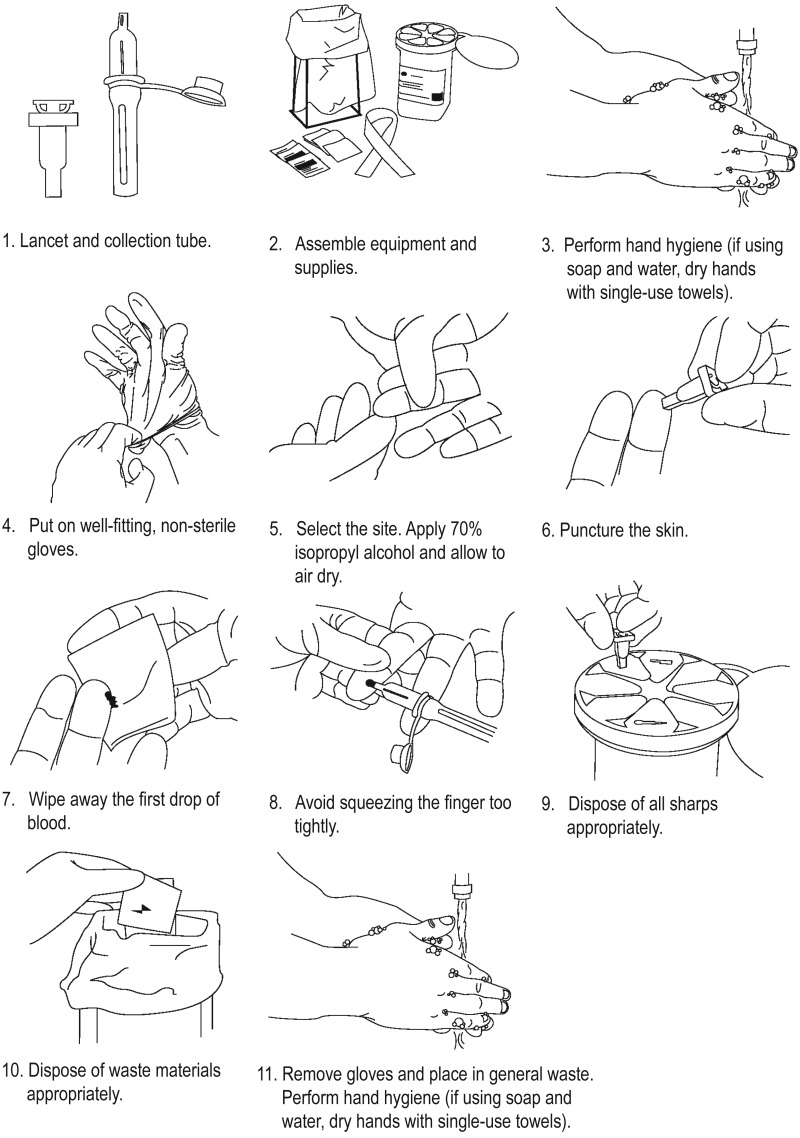
Figure 7.1Capillary sampling
What antiseptic should the phlebotomy technician use to collect a blood culture?
To help ensure accurate test results, the specimen should be brought to the laboratory for testing within 1 hr 2 hr (1 hr is preferred). Clean the venipuncture site with an antiseptic that does not contain alcohol, such as chlorhexidine gluconate.Which of the following action should I phlebotomy technician take when preparing a peripheral blood smear?
Phlebotomy Practice.Which of the following should be the first step before entering a patient's room to perform a blood collection?
Assemble equipment. ... . Identify and prepare the patient. ... . Select the site. ... . Perform hand hygiene and put on gloves. ... . Disinfect the entry site. ... . Take blood. ... . Fill the laboratory sample tubes. ... . Draw samples in the correct order..Which of the following action by a phlebotomy technician can result in a grossly Hemolyzed specimen?
Hemolysis resulting from phlebotomy may be caused by incorrect needle size, improper tube mixing, incorrect filling of tubes, excessive suction, prolonged tourniquet, and difficult collection. Tải thêm tài liệu liên quan đến nội dung bài viết A patient who has diabetes states that he prefers to be drawn on the inside of his wrist Reply
Reply
 6
6
 0
0
 Chia sẻ
Chia sẻ
Chia Sẻ Link Cập nhật A patient who has diabetes states that he prefers to be drawn on the inside of his wrist miễn phí
Bạn vừa tìm hiểu thêm tài liệu Với Một số hướng dẫn một cách rõ ràng hơn về Video A patient who has diabetes states that he prefers to be drawn on the inside of his wrist tiên tiến và phát triển nhất và Chia Sẻ Link Cập nhật A patient who has diabetes states that he prefers to be drawn on the inside of his wrist miễn phí.